Offer
Provide additional details about the offer you're running.
Written by Dr Leila Masson
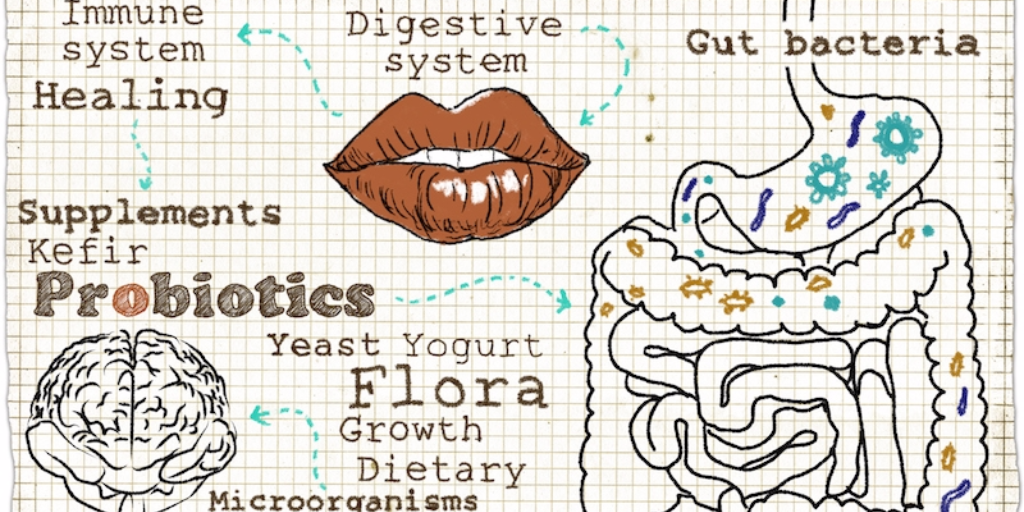
There has been an increasing amount of talk about the connection between our gut flora and disease.
Gut Flora is Linked to Mood…
Recently the research has widened to include the effect on behaviour, mood and feelings. Two recent studies reflect the important role the gut-brain connection plays in children.
In this first study, scientists found that toddlers with the highest variety of gut bacteria were more likely to be happy, curious, sociable and impulsive (I imagine in a positive way!). In boys, extroverted personality traits were associated with the abundance of specific microbes (click the link below to find out which ones).
Healthy humans have up to 500 different species of bacteria, many viruses, and even parasites in their guts. Our modern lifestyle, however has a negative influence on our gut flora: it reduces the variety of the flora and this allows overgrowth of disease-causing bugs. So what can we do to help our children grow a healthy gut flora?
In the second study children with autism received faecal transplants. This resulted in improvements in their gastrointestinal problems and their autism behaviours.
Integrative and functional doctors have been addressing gut issues in children with autism for years and found that as the diarrhoea or constipation is resolved, the children became more interactive, less aggressive, happier, and even spoke and communicated more.
Autism guidelines in the US and NZ recommend that every child on the autism spectrum be assessed, and if needed, treated for gastrointestinal problems, such as inflammation, constipation, and diarrhoea.
The gut flora of children with autism is in general quite different from neurotypical (normal) children. They have:
These clostridia produce a chemical called propionic acid, which gets absorbed into the bloodstream and can reach the brain. When researchers injected this into mice’s brains, the mice started to act autistic. And when children with autism and clostridia were treated with antibiotics for the clostridia, their behaviour became more neurotypical.
I find this fascinating. Microbiome research is booming right now and scientists are investigating the connection of an abnormal gut flora and various diseases, including:
The gut flora appears to play a role in these and many other diseases which were never thought to be associated with the gut.
This means that we need to do anything–and–everything we can to help our children grow a healthy gut flora with a great variety of bacteria. In the United States and in New Zealand the guidelines for treating children with autism includes the recommendation to assess each child on the spectrum for gastrointestinal problems, as the rate is so high. The pain and inflammation caused by the gastrointestinal issues can result in behaviour problems that cannot improve with behavioural approaches, but only with appropriate treatment of the gut issues and pain. Hopefully, Australia will follow suit soon and include this recommendation in the national autism guidelines.
Dr Leila Masson is an integrative paediatrician who combines Western medicine with a nutritional, environmental and biomedical approach to help her patients attain optimal health.
Article 1 Toddler tantrums may be due to their gut flora
Article 2 Autism symptoms improved with faecal transplants